Learn about the history and future of resuscitation (CPR)
Post - 7th July 2015
The common memory that people have of resuscitation (CPR) training is that it seemed to continually change. This is true and reflects one of the issues with CPR over the years in that it has suffered from the influence of unproven theory of how CPR works. While the concept is quite old, it was not really till late 2005 at the meeting of the International Liason Committee on Resuscitation (ILCOR) that the review of real evidence stabilised the frequent changes in CPR practice. There is still much to improve in CPR (particularly in Australia) where there is low understanding of CPR, poor availability of defibrillators in the community and basic CPR guidelines that fall short of international best-practice. In this discussion, I will try to avoid arguing about "percentage survival" as this definition as well as being subjective it is also not accurately known, particularly in Australia, where there is no centralised data for this analysis. What we do know is that a victim's heart stopping effective function is the worst thing that can happen to them and it probably won't ever start again, regardless of our best efforts. In adults, of the 33,000 victims of cardiac arrest each year, it is probably in the order of 5-10%, but probably closer to 5% overall. On a more positive note, we will look at which measures have shown an improvement in survival and which ones haven't.
So let's start our CPR journey in 1776 where the Royal Humane Society in England made recommendations about CPR that were both impractical and rather uncomfortable for the poor victim.
So let's start our CPR journey in 1776 where the Royal Humane Society in England made recommendations about CPR that were both impractical and rather uncomfortable for the poor victim.
"It is necessary to immediately stimulate the vital factors reactivating the lungs and the intestines. Then air is blown directly into the mouth of the patient and tobacco fumes are injected into the anus, at the same time keeping the body warm through rubbing performed with hot cloths or salt, or flannel soaked in brandy or rum or other strong alcoholic or spirituous liqueurs; the sense of smell is stimulated by applying spirit of volatile salt or ammoniac in the nostrils, which must be smeared on the temples to stimulate the head nerves; both throat and nostrils are tickled with a feather to reactivate the functions of the digestive apparatus inducing vomit and sneezing."
Royal Humane Society 1776
Many techniques over the years have involved rocking and manipulating victims to stimulate their circulation or breathing. At one stage, the Ambulance in NSW used carbon dioxide to ventilate victims in cardiac arrest because the "latest thinking" was that CO2 would stimulate breathing.
If we take our story to 1927, in the silent movie days, when a "breakthrough" in CPR was released by the United States Public Health Service that promised successful revival of a victim.
So after all these wacky theories, what changed in 2005 and led to changes in Australia in March 2006? Well ILCOR 2005 discovered three important things about CPR, that:
- Compressions to a victim's chest while the most important part of CPR, does not replicate the heart's function by pumping blood around the victim's body. Instead rather the pressure on the chest increases the pressure inside the chest and blood that is pooled in large vessels in the chest (including the heart chambers and the aorta which is the main large vessel coming out of the top of the heart). This pressure forces the blood in the heart and other vessels involved away from the chest. This means that much deeper and faster compressions where needed.
- The full effect of this pressure in compressions is not immediate and takes several compressions to establish, however once stopped, the blood movement stops almost instantaneously. This meant that compressions should be interrupted as little as possible.
- Compressions also result in "passive ventilation" i.e. the pressure forces some air out of the lungs and when released, air is drawn back into the lungs. When measured the amount of air forced in and out during this process is more than half the normal required amount for a conscious healthy victim (around 300-400ml in and adult). This meant that the victim was already receiving some good ventilation with just compressions. This also meant that ratios of compressions to ventilation could be increased to 30 compressions to 2 ventilations. However, at the next meeting of ILCOR in 2010 new evidence would recommend that is some instances ventilations could be omitted altogether.
One of the other, more fundamental things changing in CPR was the realisation that this was a technique that could be applied with very little training. Many organisations who had a vested interest in making CPR training seem complicated and costly resisted this change in attitude and understanding of CPR. This trend of simplifying CPR has continued and we will see that the least complicated techniques were actually the ones that made the real difference in survival.
Then at the ILCOR meeting of 2010 there was a surprise finding from research on arrests since 2005 which indicated that "in some circumstances the inclusion of ventilations in resuscitation attempts was producing worse outcomes". This news meant that the reduction in the emphasis on ventilations and the focus on compressions was showing that ventilations were in some circumstances even less important. From this central finding emerged two clear recommendations:
These findings resulted in a positive change in focus of bystander CPR in the US and Europe to the concept of "hands only" (compression only) CPR as the recommended method for bystander CPR and that ventilations are really only for emergency responders when they arrive. This change not only resulted in more people being willing to attempt CPR but meant that valuable time was not being wasted with measures that did not improve outcomes and focused the public on good compressions.
Then at the ILCOR meeting of 2010 there was a surprise finding from research on arrests since 2005 which indicated that "in some circumstances the inclusion of ventilations in resuscitation attempts was producing worse outcomes". This news meant that the reduction in the emphasis on ventilations and the focus on compressions was showing that ventilations were in some circumstances even less important. From this central finding emerged two clear recommendations:
- In victims who suffered a Sudden Cardiac Arrest (SCA) which is the most common form of arrest, the inclusion of ventilations in the initial CPR actually led to slightly poorer outcomes.
- In victims who have suffered a Hypoxic Arrest (where there is a low availability of oxygen that leads to a cardiac arrest e.g. drownings, chokings, strangulations i.e. almost all cardiac arrests in children, the inclusion of ventilations in the initial resuscitation was beneficial.
These findings resulted in a positive change in focus of bystander CPR in the US and Europe to the concept of "hands only" (compression only) CPR as the recommended method for bystander CPR and that ventilations are really only for emergency responders when they arrive. This change not only resulted in more people being willing to attempt CPR but meant that valuable time was not being wasted with measures that did not improve outcomes and focused the public on good compressions.
Post - 17th July 2015
So what are the current BLS recommendations in Australia and what should they look like if we are to improve outcomes in cardiac arrest?
The biggest single biggest improvement in survival that we can achieve i.e. <10% presently to up to 75% is if defibrillation is delivered within 3 minutes of the arrest with good compressions., The only way to achieve this target is to have a wider availability of AEDs in the community. This of course still relies on good compressions. The fact is that in the case of Sudden Cardiac Arrest (SCA), being the most common type of cardiac arrest worldwide, the only two measures that make any significant difference in the initial management are:
Good compressions - considering a UK study showed that less than 42% of the adult population including health professionals are able to achieve satisfactory chest depth, this is harder to do and sustain than most people think). We shall examine this issue later.
Early Defibrillation - if we are waiting for an Ambulance for this we will be disappointed. Average NSW Ambulance response times in metropolitan areas are around 8 minutes, well outside the ideal of less than 3 minutes. This Ambulance response time also assumes that the Ambulance was called at the very moment the patient had the cardiac arrest and the crew was already in their vehicle and the crew was able to use the defibrillator by jumping from the vehicle as it arrives and simultaneously placing the pads on the patient's chest and delivering a shock.
So what are the current BLS recommendations in Australia and what should they look like if we are to improve outcomes in cardiac arrest?
The biggest single biggest improvement in survival that we can achieve i.e. <10% presently to up to 75% is if defibrillation is delivered within 3 minutes of the arrest with good compressions., The only way to achieve this target is to have a wider availability of AEDs in the community. This of course still relies on good compressions. The fact is that in the case of Sudden Cardiac Arrest (SCA), being the most common type of cardiac arrest worldwide, the only two measures that make any significant difference in the initial management are:
Good compressions - considering a UK study showed that less than 42% of the adult population including health professionals are able to achieve satisfactory chest depth, this is harder to do and sustain than most people think). We shall examine this issue later.
Early Defibrillation - if we are waiting for an Ambulance for this we will be disappointed. Average NSW Ambulance response times in metropolitan areas are around 8 minutes, well outside the ideal of less than 3 minutes. This Ambulance response time also assumes that the Ambulance was called at the very moment the patient had the cardiac arrest and the crew was already in their vehicle and the crew was able to use the defibrillator by jumping from the vehicle as it arrives and simultaneously placing the pads on the patient's chest and delivering a shock.
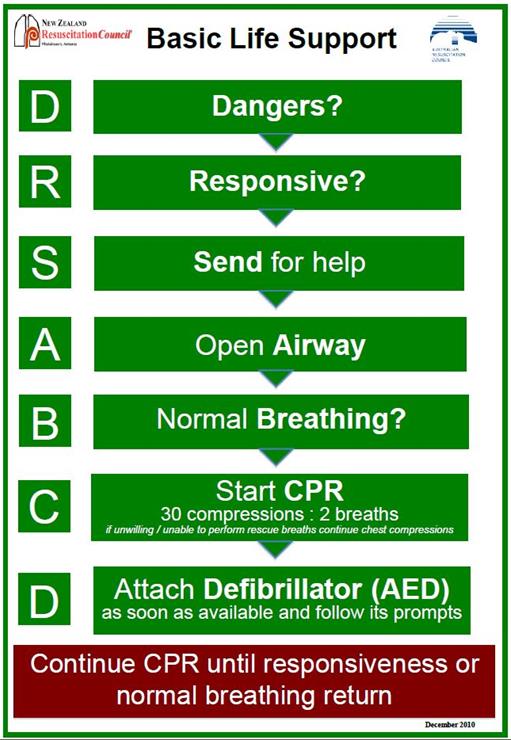
What you will notice is that their is a sequencing that places more importance on the management of the patient's airway and ventilations for patients, with the AED at the bottom of the chart. Despite a caveat that the rescuer is "unwilling or unable to performs rescue breaths" they can be omitted; ventilations and airway management are still taught as necessary and are a requirement of CPR certification in Australia, for all types of arrests i.e. CPR certification means you are presumably able (and should) include ventilations in resuscitation attempts.
Whilst ventilations are important in hypoxic arrests (as we discussed in my first post), in the first instance in SCA these may make little difference to outcome. A similar problem is also present in the appearance of "Open Airway" as a priority in the guideline. This presumes that all patients are going to receive ventilations (in which case the presence of vomit or solids is usually the only reason to clear an airway) and that a high proportion of patients may have airway obstructions, in which case the application of compressions is the recommended treatment anyway.
In a future post I will look at the lack of evidence around the ARC recommendations on the management of airway obstructions in the conscious patient.
Whilst ventilations are important in hypoxic arrests (as we discussed in my first post), in the first instance in SCA these may make little difference to outcome. A similar problem is also present in the appearance of "Open Airway" as a priority in the guideline. This presumes that all patients are going to receive ventilations (in which case the presence of vomit or solids is usually the only reason to clear an airway) and that a high proportion of patients may have airway obstructions, in which case the application of compressions is the recommended treatment anyway.
In a future post I will look at the lack of evidence around the ARC recommendations on the management of airway obstructions in the conscious patient.
Post 18th August 2015
So considering how important compressions are in resuscitation attempts, what are good compressions and how does the average person achieve these?
In one of my previous posts, we learnt that only 42% of the adult population can achieve adequate depth of compression on an adult patient, that includes health professionals. This figure is often news to health professionals, who always perceive that prior training or actual clinical experience necessarily means that they are capable of achieving satisfactory compressions. The truth is less than half of us are actually able to achieve and maintain "good compressions".
So what is the "good compression" doing in cardiac arrest, and why is it so important in resuscitation? In my 7th July 2015 post, I set out the findings of ILCOR in regard to the effects of chest compressions however, there is an additional reason why "good compressions" are essential in resuscitation, regardless of the availability of a defibrillator.
Research indicates that another function of initial chest compressions is to ensure that the heart chambers are relatively normal in size, to allow effective pumping of the heart muscle if and when heart function returns. Once the circulation ceases in a patient, there is obviously no blood leaving the heart to perfuse the vital organs and vessels of the body. However, after circulation ceases a more troubling process happens, whereby the vessels of the body as they relax, allow a slow oozing of old venous blood (high in carbon dioxide and low in oxygen) back into the non-functional heart. As a result, the heart rapidly increases in size. This increase in the heart's size can be 60% more than its original size.
So considering how important compressions are in resuscitation attempts, what are good compressions and how does the average person achieve these?
In one of my previous posts, we learnt that only 42% of the adult population can achieve adequate depth of compression on an adult patient, that includes health professionals. This figure is often news to health professionals, who always perceive that prior training or actual clinical experience necessarily means that they are capable of achieving satisfactory compressions. The truth is less than half of us are actually able to achieve and maintain "good compressions".
So what is the "good compression" doing in cardiac arrest, and why is it so important in resuscitation? In my 7th July 2015 post, I set out the findings of ILCOR in regard to the effects of chest compressions however, there is an additional reason why "good compressions" are essential in resuscitation, regardless of the availability of a defibrillator.
Research indicates that another function of initial chest compressions is to ensure that the heart chambers are relatively normal in size, to allow effective pumping of the heart muscle if and when heart function returns. Once the circulation ceases in a patient, there is obviously no blood leaving the heart to perfuse the vital organs and vessels of the body. However, after circulation ceases a more troubling process happens, whereby the vessels of the body as they relax, allow a slow oozing of old venous blood (high in carbon dioxide and low in oxygen) back into the non-functional heart. As a result, the heart rapidly increases in size. This increase in the heart's size can be 60% more than its original size.
As you can see this swelling of the heart is quite dramatic and so emptying of the heart is an important role for compressions during resuscitation as it keeps the heart relatively empty of blood so that if a normal heart rhythm is restored, the heart muscle is once again able to pump blood. Without compressions early (regardless of a defibrillator), the heart would find it very difficult (if not impossible) to pump naturally when it is distended with blood. So basically compressions to a patient's chest perform four function during resuscitation:
As we said earlier, we need to ask the question what are "good compressions' and how can we achieve them and sustain them in resuscitation. To answer that question, let's have a look at the elements that influence successful compressions:
Method - The next determinate is the method of compressions the rates, ratios and depths. It is recognised by the international resuscitation community, that rates and depths of compressions are crucial in ensuring that the positive effects are realised.
Before we continue let's clear up one of the common myths people rely on for estimating the depth of compressions. The mantra often spouted is that to estimate the depth of compression on any patient a rescuer need only to push down a 1/3 of the depth of the patient's chest. There are a few problems with this theory:
Whilst it is possible to achieve 1/3 in children and babies (paediatrics), there is an easier way for the rescuer to calculate this. An approximation for paediatrics is based on a simple anatomical fact. Up to the age of approximately 6 years of age, a child's chest width and chest height are about equal. So all the rescuer has to do to calculate depth is to divide the child's chest width into thirds, this distance is then the approximate depth you need to push down. After around 8 years old and up to an adult the width of a patient's chest is twice the depth of their chest. So if we were to measure from the middle (sternum) to the side of the patient can be divided into thirds to calculate depth.
Technique - The technique of compressions does make a difference as to how effective, sustainable and difficult it becomes. The first element to tackle is hand grip (or digit position in babies). Most trainers and web, describe the "interlocking fingers" technique. (see image)
- Compressions initially empty the heart of old venous blood that pools there after the heart has stopped.
- Compressions of the chest decrease the size of the chest and increase the internal pressure, this acts to pressurise blood in large vessels in the chest, like the aorta (the large vessel that comes from the top of the heart) and this blood is forced away from the chest and returns when the compression is released. Blood is not circulated by compressing the heart and squeezing blood from the squashed heart through the circulatory system.
- Compressions force some blood in the aorta into the carotid and coronary arteries (which supply the brain and heart muscle with blood) and so a small amount of perfusion takes place, of these important organs.
- Compressions create passive ventilation (in the order of 300-400ml of TV). In the case of a Sudden Cardiac Arrest (SCA) this passive ventilation is adequate for resuscitation attempts by lay rescuers.
As we said earlier, we need to ask the question what are "good compressions' and how can we achieve them and sustain them in resuscitation. To answer that question, let's have a look at the elements that influence successful compressions:
- The strength and mass of the rescuer.
- The method used i.e what rates, ratios and depths are best.
- The technique used i.e. how compressions can be most effectively done on patients of different size and within the limitations of the rescuer.
Method - The next determinate is the method of compressions the rates, ratios and depths. It is recognised by the international resuscitation community, that rates and depths of compressions are crucial in ensuring that the positive effects are realised.
Before we continue let's clear up one of the common myths people rely on for estimating the depth of compressions. The mantra often spouted is that to estimate the depth of compression on any patient a rescuer need only to push down a 1/3 of the depth of the patient's chest. There are a few problems with this theory:
- On an Adult 1/3 of the chest depth is not achievable. The most depth achievable on an actual adult is approximately 15-20% of the chest depth (although 1/3 may be achievable on a typical Adult BLS manikin)
- The second issue is how does a rescuer measure 1/3 of the chest depth when they are viewing it from the top as they do compressions. Either someone else has to evaluate the chest depth or the sole rescuer has to have an out-of-body experience and watch themselves doing their own compressions from the side to calculate 1/3.
Whilst it is possible to achieve 1/3 in children and babies (paediatrics), there is an easier way for the rescuer to calculate this. An approximation for paediatrics is based on a simple anatomical fact. Up to the age of approximately 6 years of age, a child's chest width and chest height are about equal. So all the rescuer has to do to calculate depth is to divide the child's chest width into thirds, this distance is then the approximate depth you need to push down. After around 8 years old and up to an adult the width of a patient's chest is twice the depth of their chest. So if we were to measure from the middle (sternum) to the side of the patient can be divided into thirds to calculate depth.
Technique - The technique of compressions does make a difference as to how effective, sustainable and difficult it becomes. The first element to tackle is hand grip (or digit position in babies). Most trainers and web, describe the "interlocking fingers" technique. (see image)
This technique was introduced many years ago in an attempt to reduce rib fractures by holding the fingers off the chest. The truth is, the force of compressions is exerted through the ball of the lower hand and regardless of how many fingers are in contact with the chest it will not change the occurrence of rib fractures; they are just part of pushing a patient's chest down 60 mm and generally don't cause any additional problems. The real problem with this technique is that what the rescuer is doing in using this technique is hyperextending the wrist of the lower hand and this leads to not just wrist pain but in some instances wrist damage. A better technique is the "locked wrist" technique. In this technique, the thumb and index finger of the upper hand grip around the wrist of the lower hand (at the level of that little bump on the little finger side on the back of your wrist). In this position, the wrist of the lower hand is supported, braced and protected during compressions.
The other important element in good compressions is making the best use of your body mass. The way to do this with the traditional kneeling technique for an adult is to move your knees back till your thighs are vertical, with your elbows locked and pivoting from the hips rather than knees. If your knees are too close the patient then the stress will be on your erector muscles and they will fatigue quickly. If your knees are too far away you will tend to pivot at the knees rather than the hips and most of your force will be directed sideways rather than straight down. On an adult, the traditional kneeling technique is not the only way to do good compressions and for some people who a weak, light or have injuries or disabilities it is impossible/ineffective and there other techniques used successfully around the world for special situations.
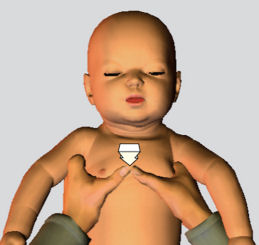
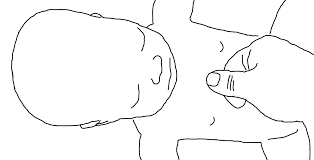
With children and babies (paediatrics), there are also a few tips to make this more effective. With young children (what looks like it is between 1 and 8 years), one hand should be sufficient but just remember that there are no rules here, so if the patient is stiff or you are getting tired, then use two hands (like an adult). For babies (look like they are under 12 months), the traditional 2 finger technique is not as effective at providing sufficient pressure change in the chest (essential for effectiveness) as other techniques used across the medical system. The best method, that is used by every neonatal ward in Australia is the 2 thumb technique. A few years ago a couple of doctors developed a third technique using two fingers but proved to be clinically superior to the traditional two finger technique and showed no increase in complications caused by compressions.
The other important element in good compressions is making the best use of your body mass. The way to do this with the traditional kneeling technique for an adult is to move your knees back till your thighs are vertical, with your elbows locked and pivoting from the hips rather than knees. If your knees are too close the patient then the stress will be on your erector muscles and they will fatigue quickly. If your knees are too far away you will tend to pivot at the knees rather than the hips and most of your force will be directed sideways rather than straight down. On an adult, the traditional kneeling technique is not the only way to do good compressions and for some people who a weak, light or have injuries or disabilities it is impossible/ineffective and there other techniques used successfully around the world for special situations.
With children and babies (paediatrics), there are also a few tips to make this more effective. With young children (what looks like it is between 1 and 8 years), one hand should be sufficient but just remember that there are no rules here, so if the patient is stiff or you are getting tired, then use two hands (like an adult). For babies (look like they are under 12 months), the traditional 2 finger technique is not as effective at providing sufficient pressure change in the chest (essential for effectiveness) as other techniques used across the medical system. The best method, that is used by every neonatal ward in Australia is the 2 thumb technique. A few years ago a couple of doctors developed a third technique using two fingers but proved to be clinically superior to the traditional two finger technique and showed no increase in complications caused by compressions.
The final technique for babies is to do CPR with the child on your arm. In this method, the infant is laid on your forearm face-up with the head cradle in your hand to maintain the neutral head position. The baby's legs should fall each side of your arm i.e. the baby's crutch is up against the inside of your elbow. If your arm isn't long enough then just tuck both legs underneath your armpit and squeeze the legs to hold securely. In this position, the baby can be rolled to clear vomit, compressions using the new two-finger technique and ventilations can be performed. The benefit of this technique is that you are now fully mobile to go to help while continuing resuscitation. In remote areas, you could even continue CPR while someone else drives to meet the Ambulance en-route.
Post 10th February 2016
BLS - Summary of Changes December 2015
BASIC LIFE SUPPORT GUIDELINES
SUMMARY OF CHANGES
"The only change to the ANZCOR BLS guidelines in light of the release of the ILCOR Consensus on Science and Treatment Recommendations is related to rate of chest compressions and this has changed from “approximately 100” to “100 to 120 compressions per minute”. ANZCOR acknowledges that compression rates will vary between and within providers and there is evidence that survival rates are optimised at compressions rates of 100-120 compressions per minute. There is some evidence that compressions rates less than 100 or greater than 140 compressions per minute are associated with lower rates of survival.
The recommendations regarding depth of compression are unchanged however ANZCOR does acknowledge evidence suggesting detriment with compression depths greater than 6cm. In making the decision not to change our current recommendations (sternum should be depressed approximately one third of the depth of the chest with each compression. This equates to more than 5cm in adults, approximately 5cm in children and 4 cm in infants), ANZCOR has taken the view that the clinical reality of being able to tell the difference between 5 or 6 cm and adjust compressions accordingly is questionable. Inadequate compression depth is definitely associated with poor outcomes. ANZCOR has elected not to put an upper limit on compression depth as the risk of too shallow compressions outweighs the risk of compressions that are too deep."
BLS - Summary of Changes December 2015
BASIC LIFE SUPPORT GUIDELINES
SUMMARY OF CHANGES
"The only change to the ANZCOR BLS guidelines in light of the release of the ILCOR Consensus on Science and Treatment Recommendations is related to rate of chest compressions and this has changed from “approximately 100” to “100 to 120 compressions per minute”. ANZCOR acknowledges that compression rates will vary between and within providers and there is evidence that survival rates are optimised at compressions rates of 100-120 compressions per minute. There is some evidence that compressions rates less than 100 or greater than 140 compressions per minute are associated with lower rates of survival.
The recommendations regarding depth of compression are unchanged however ANZCOR does acknowledge evidence suggesting detriment with compression depths greater than 6cm. In making the decision not to change our current recommendations (sternum should be depressed approximately one third of the depth of the chest with each compression. This equates to more than 5cm in adults, approximately 5cm in children and 4 cm in infants), ANZCOR has taken the view that the clinical reality of being able to tell the difference between 5 or 6 cm and adjust compressions accordingly is questionable. Inadequate compression depth is definitely associated with poor outcomes. ANZCOR has elected not to put an upper limit on compression depth as the risk of too shallow compressions outweighs the risk of compressions that are too deep."
Post 28th May 2016
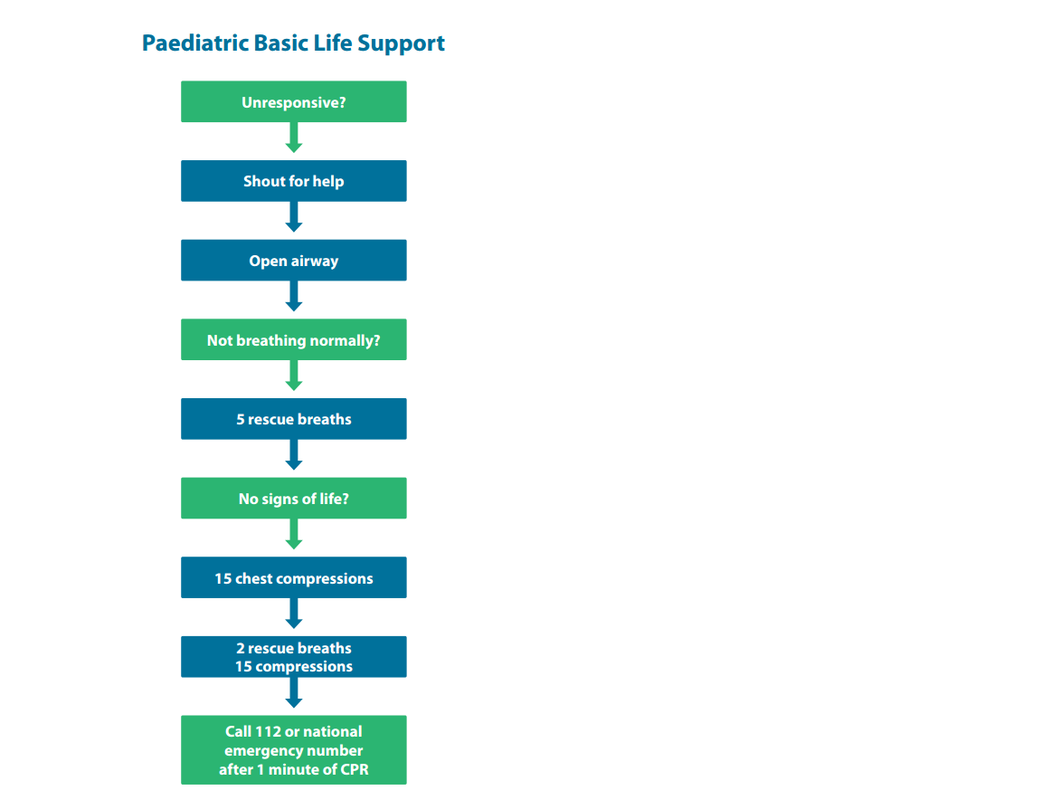
The European Resuscitation Council (ERC) has released their new guidelines, including now recommending that the BLS Guidelines for Children be the same as the ALS Guidelines (see below). This includes using the ratio of 15:2 for CPR due to the high likelihood that a peadiatric arrest will by caused by a hypoxic episode.
The European Resuscitation Council (ERC) has released their new guidelines, including now recommending that the BLS Guidelines for Children be the same as the ALS Guidelines (see below). This includes using the ratio of 15:2 for CPR due to the high likelihood that a peadiatric arrest will by caused by a hypoxic episode.
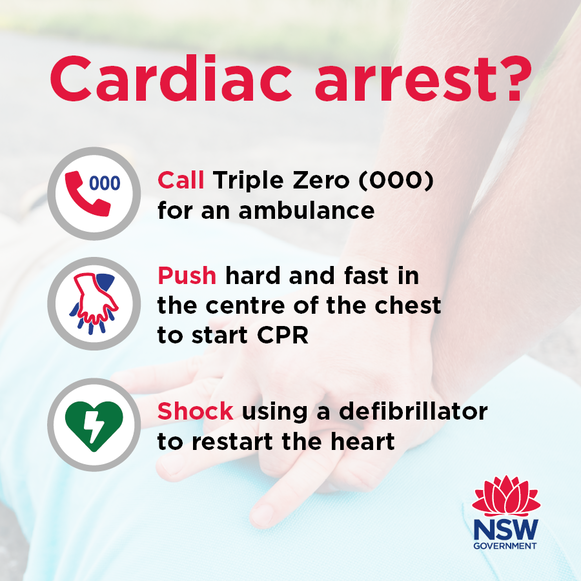
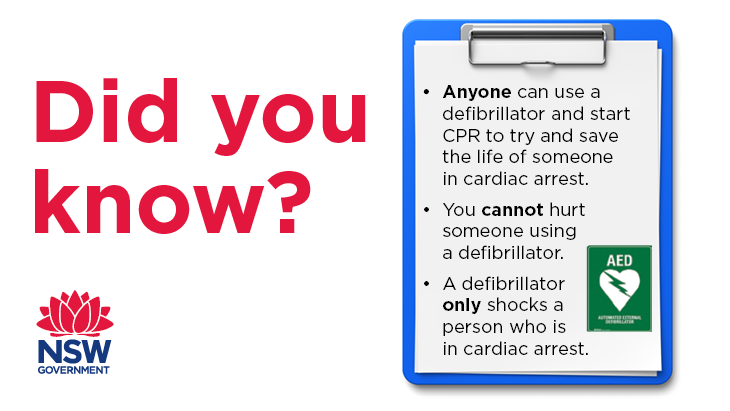
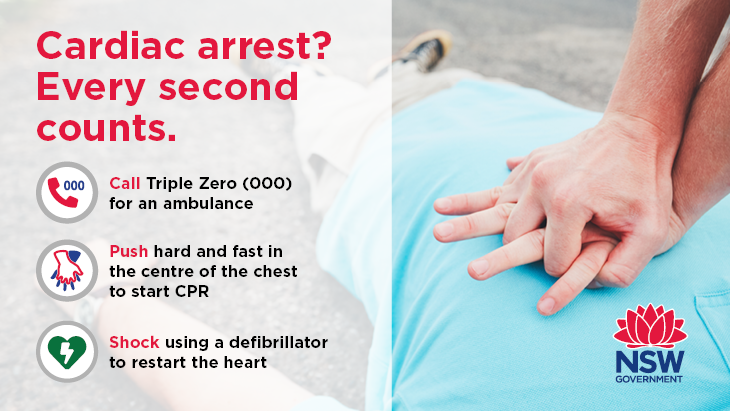
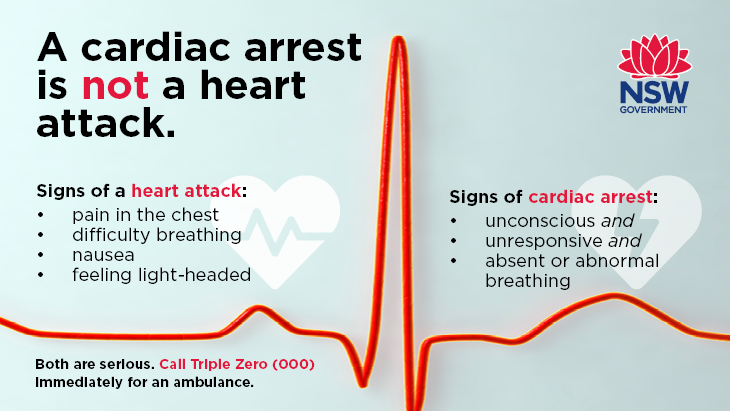
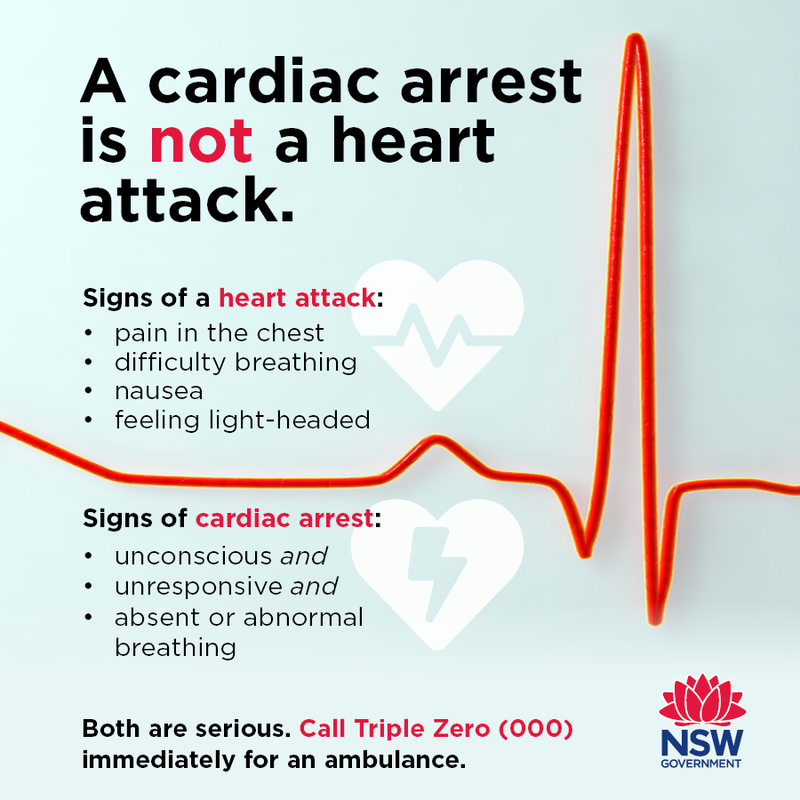
NSW Health releases new advice for initial response to cardiac arrest
After a lot of debate, lobbying and support from other groups passionate about improving cardiac arrest survival rates, NSW has changed its messaging to reflect world's best-practice for the initial response to suspected cardiac arrest. The traditional and largely redundant DRSABCD advice for the public has been replaced with a simple message that is supported by the international evidence: CALL-PUSH-SHOCK i.e. the only 3 things that have proven to improve cardiac arrest survival rates in Sudden Cardiac Arrest (SCA - 85% of all arrests). Well done NSW Health this has shown leadership and resolve to implement this regime in the face of biased resistance from certain quarters. The full suite of social media and posters are available below.